Better diet, a better lifestyle and better medicine have all greatly increased length of life around the world. The average gain globally in terms of life expectancy has been close to 25 years since 1950.[1]
Wealthier populations enjoy the highest life expectancy at birth. Someone born today in an economically advanced country can expect to live more than 80 years.[2]
While mass killers of previous centuries such as smallpox have been eradicated by vaccination, this is not the case with cancer. In many countries, including Belgium, the Netherlands, France and Australia, it is now the biggest cause of death.
While the percentage of older people in society is growing as a result of benign trends, it is evident that cancer disproportionately attacks this segment. As longevity has increased, so has cancer incidence: from 15% in 1960 to 25% today.
The risk of being diagnosed with cancer nearly doubles as we age from our 30’s to our 40’s and increases more than four times from our 30’s to our 50’s. A person in their 70’s is more than five times more likely to be diagnosed with cancer than a person in their 30’s.[3] The experts unanimously agree that the number of cancers will increase significantly in the coming years, particularly as a result of the combined effect of the increase and ageing of the world population. Nearly 40% of the population might be diagnosed with cancer during their lifetime.[4]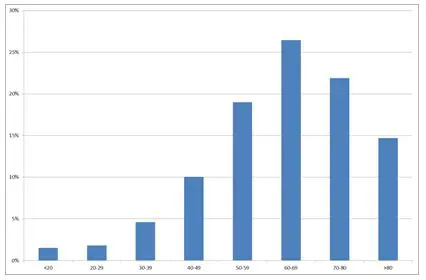
How is this possible? There are more than 100 different types of cancer and three broad sources of malignant tumours: genetic inheritance, infection, and sporadic tumour. But, in all cases, the process is the same: cellular “quality control” mechanisms become defective and the body cannot destroy the mutant cells fast enough. As we age, our capacity to repair DNA weakens: more abnormal cells raise the amount of genetic instability, which then increases the likelihood of cancer. Almost three-quarters of the genetic mutation signatures proposed for cancer are also found in ageing.[5]
Cancer cells themselves have some anti-ageing qualities. These cells boost their lifespan by busily producing telomeres, which are known to protect our DNA from destruction as shoelace caps protect the shoelaces from fraying. Ageing, on the other hand, is all about decay in the telomeres. Normally, as we age, with every cell division we lose a tiny bit of a telomere, and when this protective DNA element is lost, the cell dies. In laboratory experiments, scientists have shown that stimulating telomere production increases the lifespan of mice of different ages by 20%.[6]
A crucial element to this experiment was that cancer was not an inevitable unfortunate consequence of the anti-ageing treatment. This discovery gives us hope that we can live longer beyond the shadow of this disease.
Importantly, the remedies discovered in laboratories are not the only means of beating cancer. Although its many forms are not yet fully understood, scientists reckon 90-95% of the causal cancer risk factors are modifiable, i.e. within our power to address. These include lack of exercise, sun exposure, obesity and environmental conditions.[7] The trend against smoking – still a source of roughly one-quarter of cancer cases – is a good example of how changing habits improves life. According to the WHO, nearly a third of cancer deaths are due to those five main behavioural and dietary risk factors: "30-to-50% of cancers can currently be prevented through a better prevention policy – one that involves the reduction of risk factors and the application of existing evidence-based preventive strategies", the agency points out.
Death from cancer has been falling dramatically – by on average 18% since 1990 in richer countries. This is happening due to the lifestyle improvements supported by the efforts of national healthcare systems (e.g. the National Cancer Control Programme initiated in the Czech Republic). However, the longevity trend means that incidences will strongly continue to rise. By 2040, there will be an estimated 27.5m new cancer diagnoses, 60% more than in 2018.
Moreover, as more economies improve their standard of living, so the dual trend of rising longevity and cancer will be experienced more on continents such as Asia. Changing lifestyles, including increased calorie consumption and less physical activity, are beginning to have an influence.
Society, and healthcare systems in particular, must prepare themselves for the silver tsunami, the rising wave of older people with health conditions peculiar to their age. On the one hand, research laboratories are attempting to discover new anti-ageing therapies, e.g. tweaking the function of the telomere. On the other hand, oncology departments in hospitals will undoubtedly grow, along with attendant screening and surgical equipment sales. Medical training will tilt towards cancer treatment. Big Data will improve analysis and prognosis while smartphone apps will put some of these capabilities in the hands of patients.
Conclusion
The proliferation of pharmaceutical research, the mobilization of academic research and the dynamism of start-ups and biotechnology companies are all additional assets in the fight against cancer. Scientific and technological progress heralds the advent of more precise, personalized and, above all, more effective medicine. Increasingly sophisticated combinations of treatments will strengthen the therapeutic arsenal available to health professionals to improve survival rates and even the total recovery of patients. The promises related to the widespread use of immunotherapies and gene therapies are a source of hope for many patients. Artificial intelligence and health data will also bring new perspectives in this area. These new technologies will revolutionize the detection, treatment and management of cancer. At a minimum, they will be a valuable tool to support medical decision-making. Ultimately, all these initiatives pursue a universal objective, which we fully share at Candriam: to contribute to a healthier and longer life.
WHAT ABOUT THE YOUNG?
Cancer is not exclusively an illness of older people and not all cancers are age-related. For example, since the early 1990s, the group experiencing the fastest-growing incidence of brain cancer and leukaemia in the UK has been under 25. Absolute numbers are still low compared to older people. Nonetheless, there are unpleasant consequences of some cancer treatments, which, while they apply to all ages, affect younger sufferers earlier and for longer. In one study, 20-year-old survivors of childhood cancer were found to have the same cumulative incidence of severe, life-threatening and fatal chronic health conditions as 50-year-old siblings.[8]
BETTER SCREENING
While the causal link between population-ageing and cancer incidence seems proven, some studies qualify this statement: this increase is believed to be due in particular to progress in the field of screening, with many cases not previously detected.[9]
[1] https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5058-9
[2] Source OECD Health at a Glance 2017
[3] The Global Cancer Observatory (GCO) http://gco.iarc.fr/
[4] https://www.cancer.gov/about-cancer/understanding/statistics
[5] Alexandrov LB, Nik-Zainal S, Wedge DC, et al: Signatures of mutational processes in human cancer. Nature 500: 415-421, 2013.
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3494070/
[7] https://www.ncbi.nlm.nih.gov/pubmed/18626751
[8] Arora M , Sun C-L , Ness KK , et al . Physiologic frailty among hematopoietic cell transplantation (HCT) survivors suggests accelerated aging and is a predictor of premature mortality: a report from the Bone Marrow Transplant Survivor Study (BMTSS). Blood 2015;126:739.
[9] Cancer in France, INCa (February 2015).
